Kilili: $6.5M in Medicaid funding now available
[B]WASHINGTON, D.C.[/B]—One small change in the law means a big difference in the out-of-pocket cost for Medicaid now shouldered by the CNMI government.
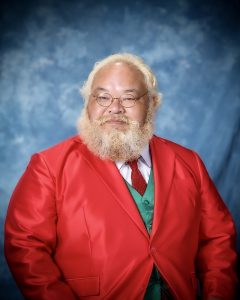
CNMI Delegate Gregorio “Kilili” C. Sablan reported from Washington that the American Recovery and Reinvestment Act, signed by the President last month, raises the cap on federal Medicaid reimbursement by 30 percent, easing the burden on the local government.
“That’s an extra $1.5 million of CNMI taxpayers’ money that has been spent for Medicaid and now can be used for other purposes,” Sablan said.
About 12,000 patients in the CNMI have the cost of their treatment paid by the Medicaid program, according to the CNMI Department of Public Health. More than half the patients are indigenous.
The annual cost of the program for the CNMI government is approximately $7.2 million.
Sablan worked alongside other insular area members of Congress to raise the federal share of the program by 30 percent in the recently passed stimulus bill.
“This increase is overdue,” said Sablan. “Federal Medicaid spending in the Northern Marianas—and all the insular areas—is below what U.S. states get. That places an undue burden on our local taxpayers to maintain this federal program.
“This stimulus funding for Medicaid will help ease that burden. It will also mean that there is extra money to help ensure adequate medical care for our population or pay for other important government services.”
A complicated formula
The federal payment to the CNMI is based on a complicated formula and the CNMI has a choice in how to use the stimulus money.
There are two limits on how much the CNMI can get:
First is the “Federal Medical Assistance Percentages.” FMAP is the percentage of a patient’s Medicaid expenses covered by the federal government. In some States the FMAP is 80 percent. But in the CNMI it is 50 percent. This means that the federal government pays 50 percent of an individual’s Medicaid expenses; and the NMI government is responsible for the remaining 50 percent of that individual’s Medicaid expenses.
Second is a cap on the overall dollars the federal government will pay for Medicaid in the NMI. The 2009 cap was $5 million. The local government is responsible for Medicaid expenses above this cap. Last year the CNMI paid $7.2 million as the local share.
The American Recovery and Reinvestment Act actually offers the CNMI a choice on how to get the new federal money.
Option one increases the FMAP percentage by 6.2 percent, so the federal government covered 56.2 percent of a patient’s bill and the CNMI covered the remaining 43.8 percent. Option one also increases the overall cap by 15 percent to $5.7 million.
Option two doesn’t change the FMAP. The federal government and the CNMI both cover 50 percent of the bill. But option two raises the cap by 30 percent to $6.5 million. That’s an extra $1.5 million to the CNMI
“It is up to the local government whether to choose option one or option two,” said Sablan. “The money is available. Now it’s their decision.” [B][I](PR)[/I][/B]